Ankle Ligament Injury & Reconstruction for Ankle Instability
Ankle Sprain
Following your ankle sprain, the ligaments on the outside of your ankle will have been either partially or completely torn depending upon the severity of the injury.
If the ligaments do not heal well, and a course of physiotherapy is unsuccessful in retraining the ‘balance’ receptors around your ankle, then you may experience ankle instability, with episodes of ‘giving way’.
This may occur with simple walking, or whilst trying to return to sport. Often patients describe a ‘lack of trust’, and modify their lifestyle around the problematic ankle, which usually means temporarily giving up sporting activity.
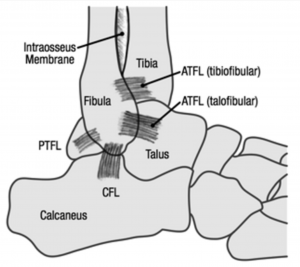
The ligaments on the outside of the ankle, when functioning well, stop the ankle from rolling inwards and sliding forward. The anterior talofibular ligament (ATFL) is most commonly injured with an ankle sprain and attaches from the fibula (outer ankle bone) to the talus (middle ankle bone), The calcaneofibular ligament (CFL), and posterior talofibular ligament (PTFL), are less commonly involved.
Diagnosis for Ankle Ligament Injury
The diagnosis is usually made from speaking to you about your injury, and performing a thorough clinical examination. After a recent ankle sprain, it will not be possible to fully test the stability of the ankle, as there will be pain and swelling.
In general, we will perform a test, called the ‘anterior draw’, which aims to assess the stability of the outer ankle ligaments. The foot is pulled forward whilst stabilising the leg and the amount of movement is compared to the other ankle. Occasionally there is a ‘clunk’ felt, indicating a very unstable ankle.
Your symptoms may also include pain, and this is very common. We will assess your ankle for signs of ankle impingement (catching of the ligaments in the ankle joint). Further investigations such as a MRI scan are usually needed to be fully informed about the cause of your ankle pain.
Treatment of Ankle Ligament Sprains and Tears
Treatment depends on the severity of the instability, the effect on your quality of life, in particular your desire to return to sport, and the presence of pain.
- Physiotherapy
This is the first line of treatment and is often very successful. This is directed at retraining the ‘balance’ fibres in the damaged ligaments, as well as strengthening the muscles around your ankle. Often you will have been treated by a physiotherapist before my assessment, but if not, I will refer you to a specialist physiotherapist, with an interest in foot and ankle problems. You can discuss the relative merits of using an ankle brace with myself and your physiotherapist. Braces can help prevent on-going giving way episodes but can be quite restrictive, and cumbersome to use.
- Podiatry
If you have a high arched foot that tilts your heel inwards, this will increase your tendency to suffer recurrent sprains. In this scenario, I will often recommend treatment from a podiatrist, and consideration to manufacturing a corrective orthotic insole for use in your shoes.
Surgery for Ankle Ligament Sprains and Tears
If your ankle continues to give way, and the above measures have been unsuccessful, then we will discuss surgery. I would recommend a minimum of 3 months with your physiotherapist, before making such a decision.
There are two types of ligament reconstruction commonly used:
My preferred surgical method is to perform an anatomic repair of the anterior talofibular and calcaneofibular ligaments via a technique called the Brostrom repair, which involves shortening the attenuated ligaments and a direct repair with suturefixation. When the anatomical repairis reinforced with the advancement of the inferior extensor retinaculum, itis called the modified Brostrom repair. When the repair is further augmented with a synthetic internal brace, this acts as a check to inversion stresses and provides reinforcement to the anatomical repair without limiting long-term inversion/eversion motion or strength.
Complications of Ankle Ligament Surgery
- Swelling: Initially the foot and ankle will be swollen and needs elevating. The swelling will disperse over the following weeks and months but will remain evident for up to 3-6 months.
- Wound healing problems: The risk of serious wound healing problems is approximately 1%. It is important to keep the foot elevated over the first 10 days to reduce the swelling and risk of wound healing problems. In rare circumstances, further surgery can sometimes be required.
- Infection: The risk of deep infection occurring is approximately 1%. You will be given intravenous antibiotics to help prevent this. It is important to keep the foot elevated over the first 10 days to reduce the swelling and risk of infection. If there is an infection, it may resolve with a course of antibiotics but may require a period of hospitalisation or rarely, further surgery.
- Nerve damage: The superficial peroneal nerve is close to the incision. This supplies sensation to the top surface of the foot. This may rarely (1%) be damaged during the surgery and this may leave a patch of numbness on the top surface of the foot. This numbness may be permanent but would not affect function.
- Deep Vein Thrombosis (DVT): This is a clot of blood in the deep veins of the leg. The risk of a clot occurring is reported as less than 1% after foot and ankle surgery which is generally substantially lower than after hip or knee surgery. Suspicion of DVT is raised if the leg becomes very swollen and painful. There are tests that can be performed to confirm/exclude the presence of a DVT. If confirmed, you will probably require treatment with a blood-thinning agent (heparin preparation).
The main concern with regards a DVT is that rarely (<1:1000 chance with foot and ankle surgery) a piece of clot can break away in the leg and travel to the lungs which is much more serious and can be life-threatening. This is called a pulmonary embolus and signs of this include chest pain and shortness of breath.
For the first 4 weeks following surgery it is likely that you will be treated with a Thrombo-prophylaxis compression stocking (TED Stocking) to minimise the risk of DVT / PE but this does not afford total protection and exercises to keep the toes and knee moving are advised, as well as remaining generally mobile. If you are concerned that the leg has become more swollen and painful (some swelling always occurs after surgery), or if you experience chest pain / shortness of breath, then you should contact the hospital, general practitioner, or accident and emergency department immediately.
Time off after surgery
In general 4 weeks off work is required for sedentary employment, 12 weeks for standing or walking work and 16 weeks for manual / labour intensive work.
Driving
You will be able to return to driving at around 8 to 10 weeks after surgery. You need to be able to make a safe emergency stop and must inform your insurance company before returning to driving.
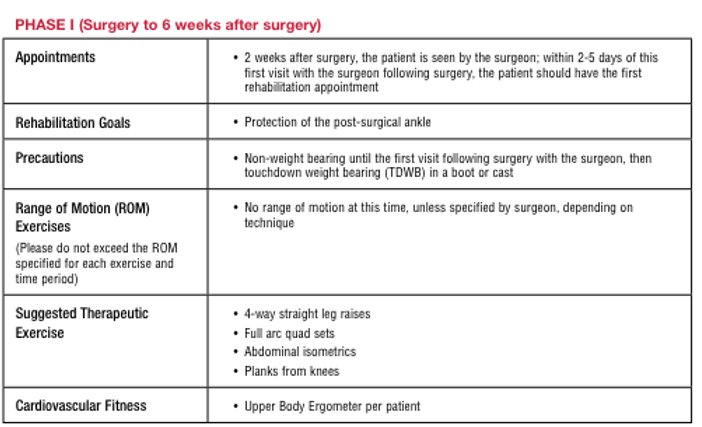
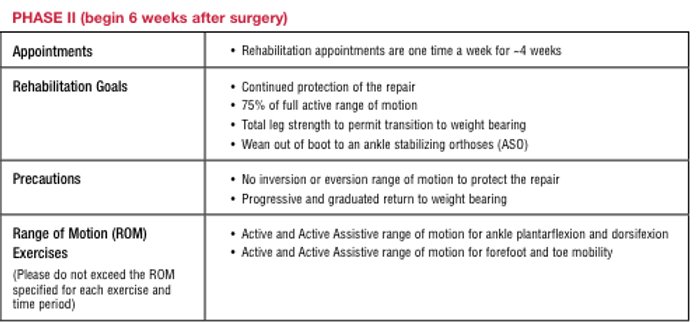
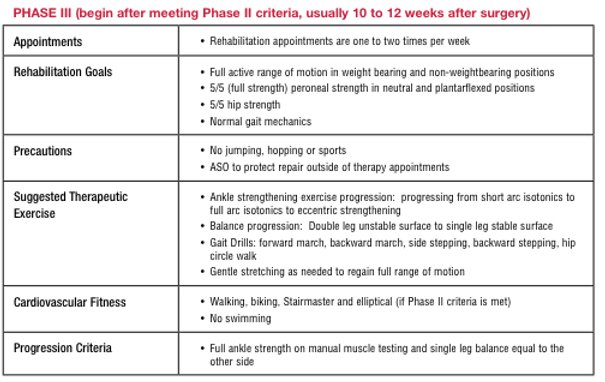
Rehabilitation after Ankle ligament Reconstruction
Surrey Orthopaedic Clinic Foot & Ankle Specialists: